DR TAHEREH FOROOGHIFAR FELLOWSHIP OF PELVIC FLOOR DISORDERS Postoperative urinary retention. - ppt download
4.5 (385) In stock

It is defined by the International Continence Society and the International Urogynecological Association as an “abnormally slow and/or incomplete micturition.
DR TAHEREH FOROOGHIFAR FELLOWSHIP OF PELVIC FLOOR DISORDERS Postoperative urinary retention.
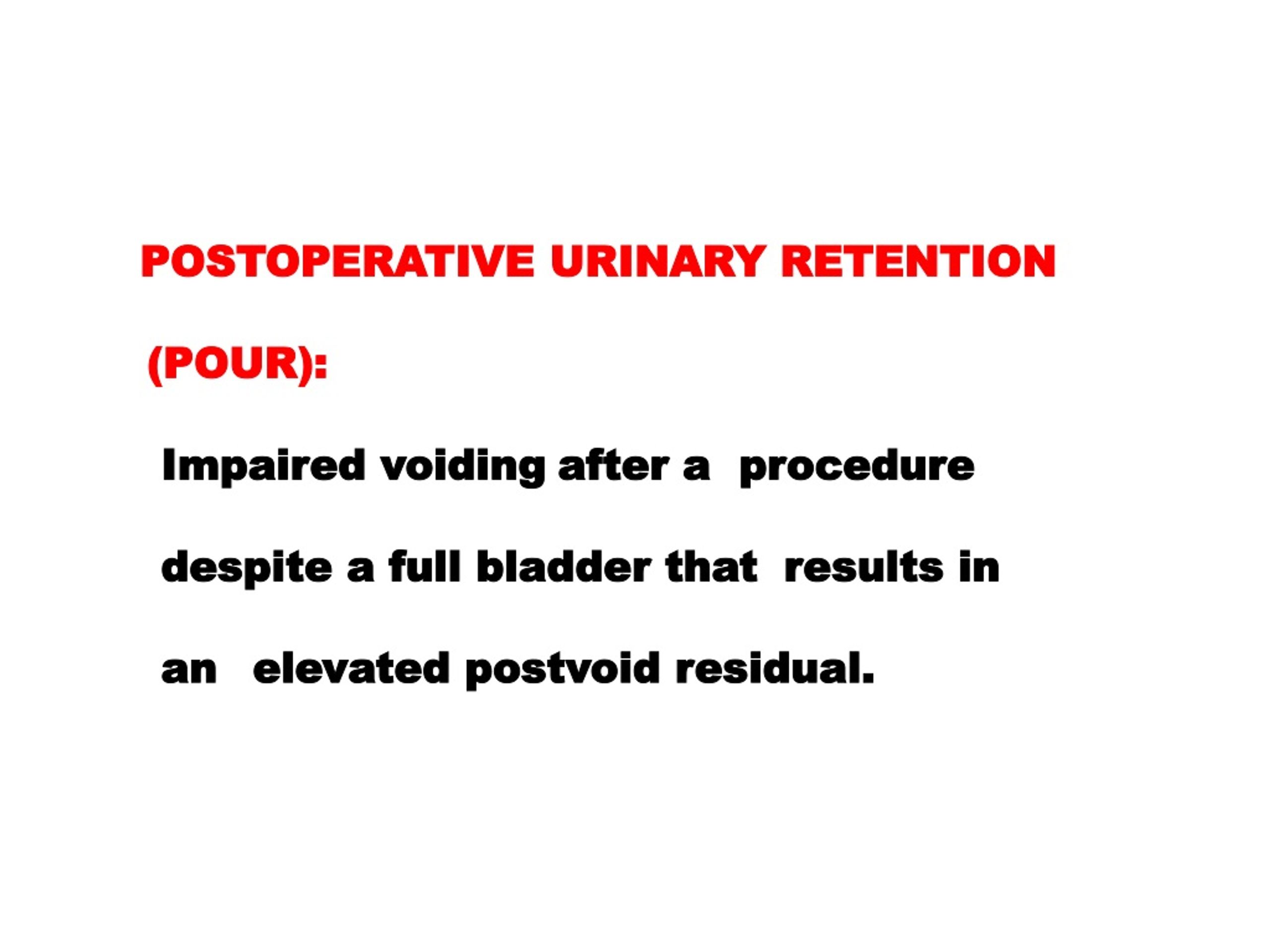
Postoperative urinary retention (POUR) refers to impaired voiding after a procedure despite a full bladder that results in an elevated postvoid residual.
It is defined by the International Continence Society and the International Urogynecological Association as an abnormally slow and/or incomplete micturition.
Pelvic surgery range 2 to 43 percent.
RISK FACTORSR ● Age over 50 years (doubles the risk of POUR) ● History of preexisting urinary retention ● Concurrent neurologic disease ● Administration >750 mL of intravenous fluid ● Duration of surgery >2 hours ● Intraoperative anticholinergic(atropine) ● Use of regional anesthesia ● History of prior pelvic surgery ● Incontinence surgery and radical pelvic surgery
Women with these risk factors for voiding dysfunction are counseled about the increased risk of POUR and may be taught clean intermittent catheterization prior to surgery.
Some risk factors can be lessened An indwelling bladder catheter: epidural anesthesia patient-controlled anesthesia vaginal pack Constipation can worsen voiding dysfunction: counseling about maintaining a bowel regimen
Specifity for elevated PVR.
CAUSES OF POUR Bladder (detrusor) dysfunction Urethral obstruction Failure of pelvic floor relaxation
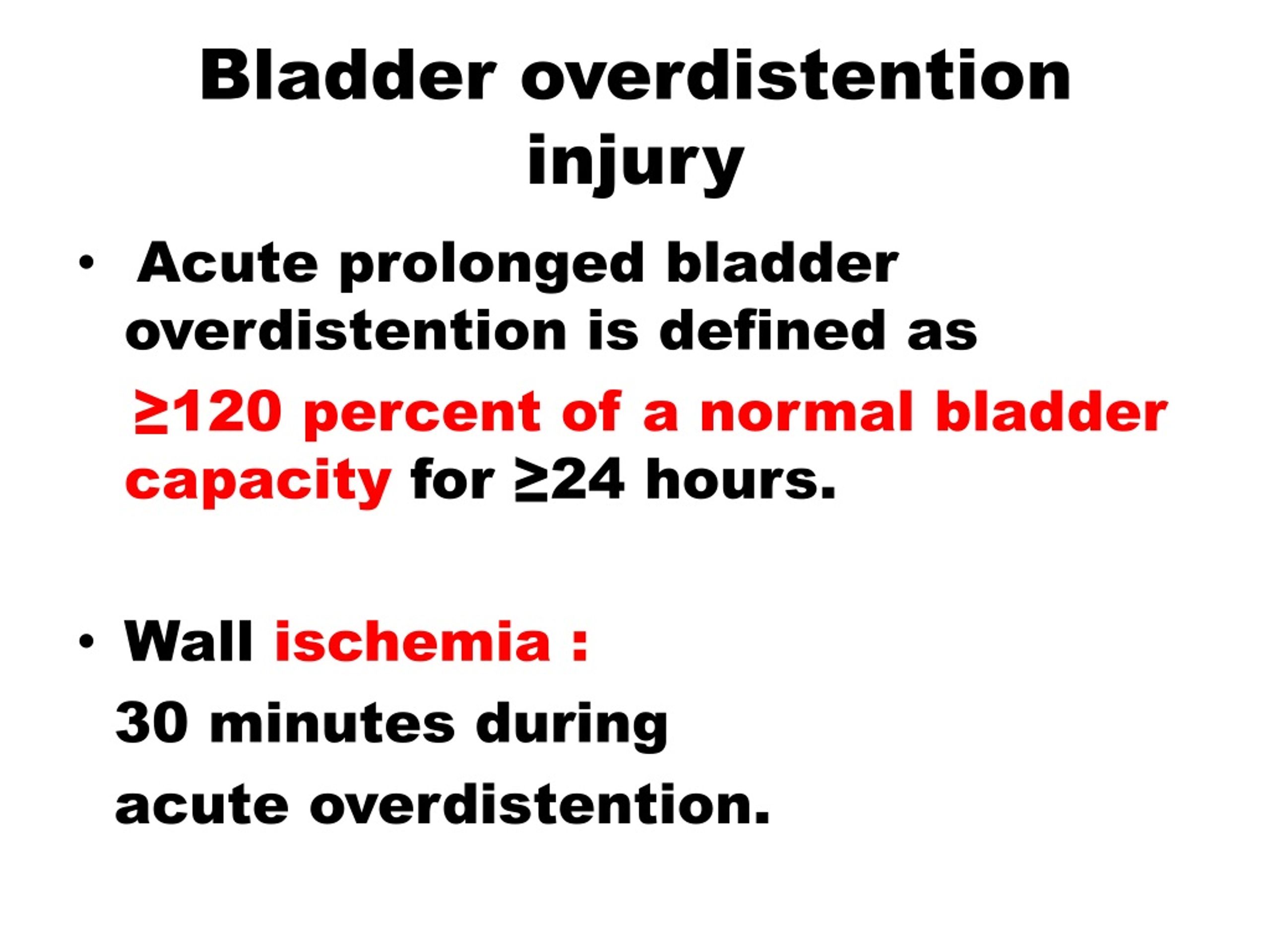
Abnormal bladder function Preexisting voiding dysfunction Anesthetic agents Nerve injury secondary to surgery Cystotomy Bladder overdistention injury Postoperative agents used for analgesia
Preexisting voiding dysfunction Aggravate with: Effects of anesthesia Surgical intervention Tissue edema, Medications Counseling prior to surgery: increased risk of POUR clean intermittent catheterization
Epidural,spinal and combined spinal/epidural Anesthetic agents.
Nerve injury secondary to surgery The main nerves at risk are: parasympathetic and sympathetic nerves in the pelvic and hypogastric plexus
total hysterectomy = supracervical hysterectomy open approach =laparoscopic approaches..
unable to void void only small volumes lack voiding sensation suprapubic pain elevated postvoid residual (PVR) abdominal fullness.
Cystotomy The differentiation cystotomy from urinary retention: Irrigating the bladder with 75 mL to 100 mL of sterile saline through a bladder catheter Attempting to withdraw the same amount of fluid cystography or cystoscopy
Ischemia and reperfusion damage to the bladder wall.
Urethral obstruction Mechanical Failure of pelvic floor relaxation
Mechanical Self-limited obstruction Sling obstruction Urethral foreign body Pelvic organ prolapse Urethral injury Constipation
Mechanical (urethral) Sling obstruction compressing the midurethra (midurethral slings) or the bladder neck (fascial slings and retropubic suspensions) Treatment: Surgical lysis of sling We do not perform urethral dilation following synthetic sling placement (increase the risk of urethral mesh erosion ).
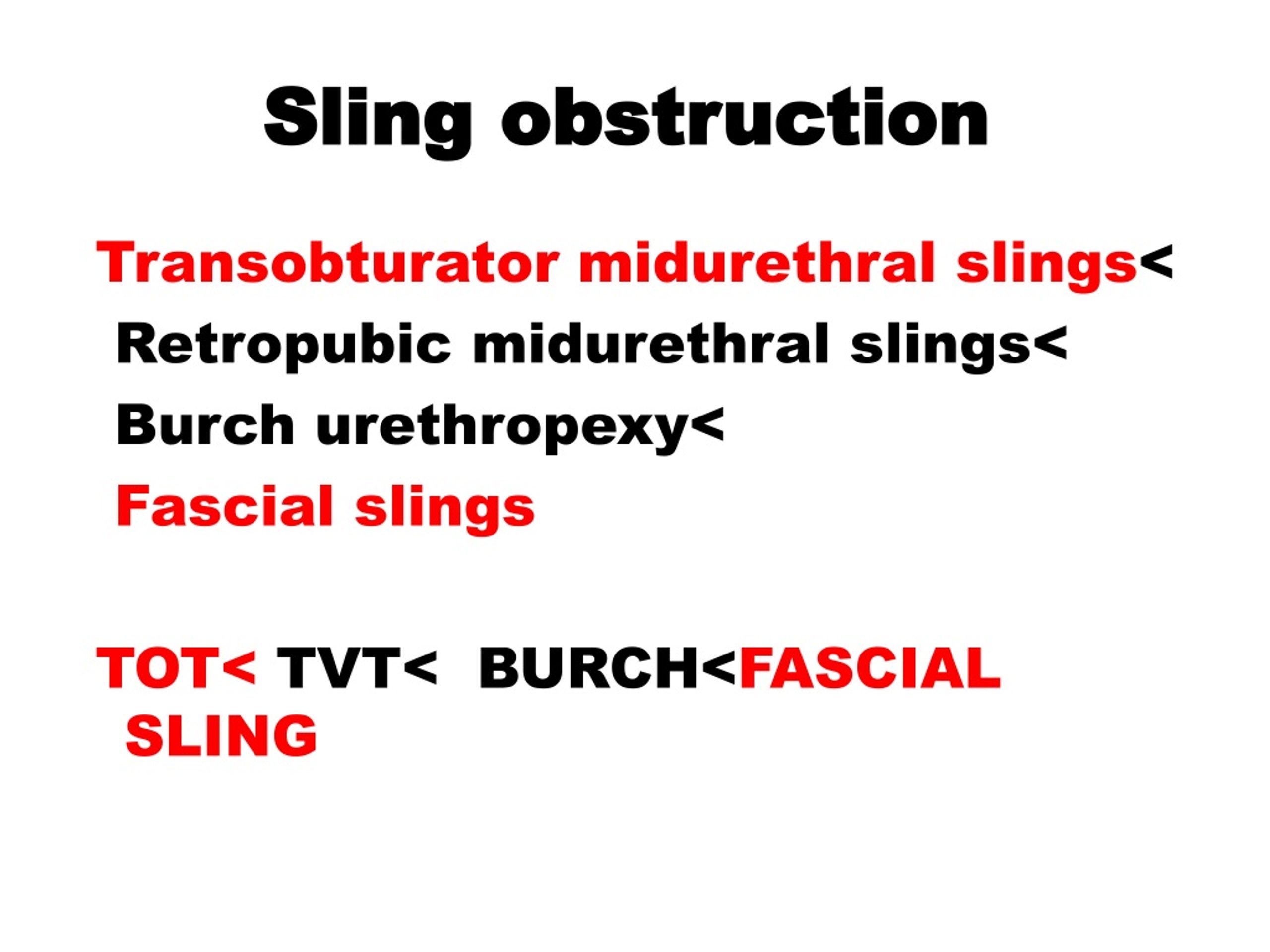
Sling obstruction transobturator midurethral slings retropubic midurethral slings Burch urethropexy fascial slings tot< tvt< burch< fascial sling
Mechanical Urethral foreign body: Possible etiologies of urethral sling erosion include : excessive sling tension postoperative transurethral dilation Cystoscopy and urethroscopy : direct visualization of the eroded sling or suture
Urethral injury Over time, foreign material in the urethra : obstructs urine flow stone formation recurrent urinary tract infection elevated PVR Requires surgical reconstruction of the urethra and removal of the causative agent.
These women typically use abdominal straining(Valsalva maneuver) to overcome the urethral outlet resistance..
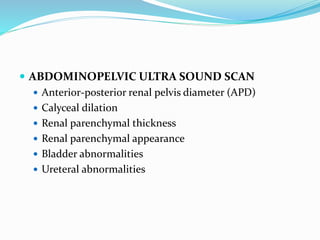
Diagnosis U/A, U/C POST VOIDING RESIDUAL VOLUME VOIDING TRIAL CYSTOSCOPY URODYNAMIC STUDY
PVR PVR of 50 mL to 100 mL is normal PVR greater than 200 mL is abnormal PVR between 100 mL and 200 mL requires clinical correlation.
Diagnosis Voiding trials performed to confirm adequate voiding and minimal postvoid residual (PVR) in patients with symptoms or risk factors for POUR.
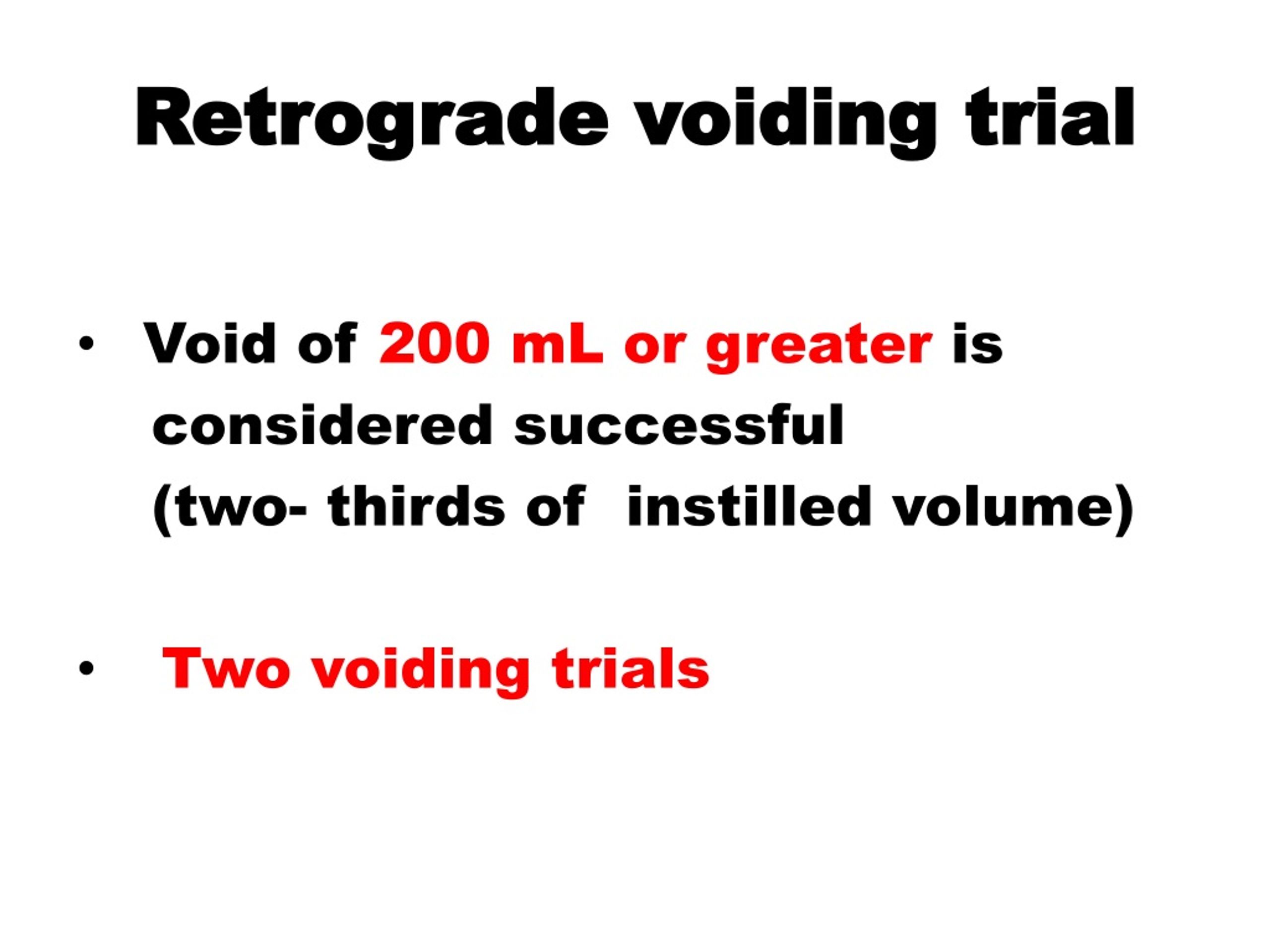
Retrograde method : more predictive of need for continued catheterization required fewer catheterizations, and took less time..
The voided volume is measured PVR :straight catheterization or ultrasound within 15 minutes of the completed void..
(total bladder volume = voided volume + PVR). Two voiding trials.
A void of 200 mL or greater is considered successful (two-thirds of instilled volume). Two voiding trials.
No evidence of obstruction CIC or indwelling bladder catheter discharg, short interval (days) follow-up in the office. retrograde voiding trial in the outpatient setting..
Persistent postoperative voiding dysfunction Examination of pelvic muscle tone Examination for prolapse Incision of midurethral sling
Examination of pelvic muscle tone Assessment of the pelvic floor tone and muscles to confirm appropriate pelvic floor relaxation Significant pain or discomfort during examination: pelvic floor physical therapy( pelvic floor muscle relaxation)
press firmly on the muscles of the patient’s right pelvic floor starting with the muscle attachment to the pubic bone at 12 o’clock and rotate to the coccyx. Assess for excessive/imbalanced muscle tone and pain at each pressure point..
Patients who have asymmetric muscle tone or frank pain are referred for pelvic floor muscle therapy..
Anterior or apical prolapse can cause bladder neck or urethral obstruction. If prolapse is found on exam pessary.
Success rates : from 86 to 100 percent.
Synthetic sling lysis one to three weeks postoperatively Fascial sling lysis one to two months following initial surgery..
Role of urodynamic testing No obstruction on exam The patient’s symptoms are inconsistent with the medical and surgical history Completely unable to void( a pressure-flow study is often helpful) Postoperative urodynamics: the bladder contractility, urethral tone, and urethral obstruction.
CIC until the patient can adequately void (>6 to 8 months) In the settings of radical hysterectomy and pelvic exenteration, the symptoms may never resolve..
COMPLICATIONS OF UNTREATED URINARY RETENTION Overdistention injury (CIC) Detrusor overactivity Overactive voiding symptoms
Reusable catheters are also available and can be used for up to four weeks..
Clean intermittent catheterization every four to six hours or urge to void, but unable catheterization If the patient is able to void a small volume, then she is instructed to perform self-catheterization (PVR) the residual urine volume is <150 mL and no longer significat symptoms discontinue catheterization
Catheterization continues: until PVRs are less than one-third of the TVV total bladder volumes are not causing overdistention..
DR TAHEREH FOROOGHIFAR Fellowship of pelvic floor disorders
Covert PUR Post void residual bladder volume of at least 150 mL with no symptoms of urinary retention..
Ethiology incidence : 0.7–4% of deliveries injury to the pudendal nerve during labour..
Risk Factors Epidural anesthesia Primiparity Instrument assisted delivery Episiotomy Prolonged labour Perineal trauma
Symptoms Asymptomatic or small voided volumes urinary frequency or urgency slow or intermittent stream hesitancy…..
Adequate analgesia (perineal pain) Constipation avoid and treatment.
Postpartum warning signs Inability to pass urine 6 hours following delivery Voided volume of less than 250 ml Women who are symptomatic of voiding dysfunction
Treatment of overt PUR Intermittent catheterization Routine use of antibiotics is not necessary Pharmacological therapies are not effective.
fill bladder slowly by drinking sufficient fluid(a glass or cupful of liquid approximately every minutes) unable to pass urine, a new catheter may be or intermittent self-catheterisation..
Voiding dysfunction after this period requires careful assessment, including a neurological examination, and is treated by intermittent self catheterisation.

DR TAHEREH FOROOGHIFAR FELLOWSHIP OF PELVIC FLOOR DISORDERS
PPT - Postoperative urinary retention PowerPoint Presentation
PPT - Postoperative urinary retention PowerPoint Presentation

Urological morbidity following pelvic surgeries
DR TAHEREH FOROOGHIFAR FELLOWSHIP OF PELVIC FLOOR DISORDERS
Management of pelviureteric junction obstruction onyeze copy

DR TAHEREH FOROOGHIFAR FELLOWSHIP OF PELVIC FLOOR DISORDERS
PPT - Postoperative urinary retention PowerPoint Presentation
Management of pelviureteric junction obstruction onyeze copy
PPT - Postoperative urinary retention PowerPoint Presentation
PDF) Postpartum urinary retention after vaginal delivery
Evaluation and Management of Voiding Dysfunction and Urinary Retention
PDF] Urinary retention in adults: diagnosis and initial management.
- cdni.llbean.net/is/image/wim/518859_34653_41?hei=1
 NILS Sportswear Ski Pants
NILS Sportswear Ski Pants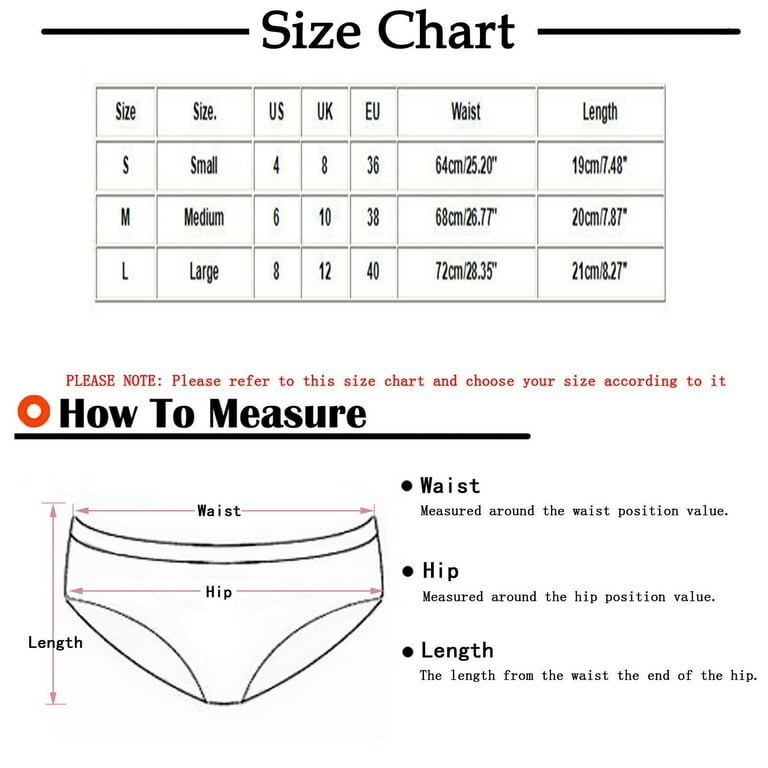 IROINNID V-Sting Underwear For Women High-Cut Sexy Lingerie Seamless Solid Color Invisible Panties
IROINNID V-Sting Underwear For Women High-Cut Sexy Lingerie Seamless Solid Color Invisible Panties Blusa tejida a crochet con motivo circular - gráficos y vídeo paso
Blusa tejida a crochet con motivo circular - gráficos y vídeo paso PUMA Brassière Femme Coton ICONICN Souris chiné
PUMA Brassière Femme Coton ICONICN Souris chiné Ethika Girls on Instagram: “Ethika ladies do it better
Ethika Girls on Instagram: “Ethika ladies do it better
